Hey there, my young and curious friends of 2024! It’s your favorite nutrition detective, Nita Sharda, here to take you on an exciting adventure into the world of diabetes management. Now, I know what you might be thinking – “Diabetes? That sounds like a grown-up problem!” But the truth is, learning about how the foods we eat can impact our health is super important, no matter what age we are.
Today, we’re going to put on our detective hats and explore how nutrition can play a key role in managing diabetes and keeping blood sugar levels in check. But before we dive in, let me make one thing clear – this is not about putting anyone on a strict diet or making them feel bad about what they eat. It’s simply about empowering you with the knowledge and tools to make informed choices about your health, now and in the future.
So, are you ready to crack the case of diabetes management with me? Let’s go!
What is Diabetes?
First things first, let’s define what we mean by diabetes. In simple terms, diabetes is a condition that affects how our bodies use and store energy from the foods we eat. When we eat foods that contain carbohydrates (like bread, pasta, fruits, and sugary treats), our bodies break those carbs down into a type of sugar called glucose, which then enters our bloodstream.
In a healthy body, a hormone called insulin helps move that glucose out of the bloodstream and into our cells, where it can be used for energy. But in people with diabetes, either the body doesn’t produce enough insulin (type 1 diabetes) or the cells become resistant to insulin’s effects (type 2 diabetes), leading to high levels of glucose in the blood.
Over time, high blood sugar levels can lead to a range of health problems, including damage to the eyes, kidneys, nerves, and heart. That’s why it’s so important for people with diabetes to carefully manage their blood sugar levels through a combination of healthy eating, regular physical activity, and medication (if needed).
The Role of Nutrition in Diabetes Management
So, how can nutrition help with diabetes management? Well, the foods we eat can have a big impact on our blood sugar levels, either causing them to spike and then crash (like after eating a sugary treat) or helping to keep them stable and within a healthy range.
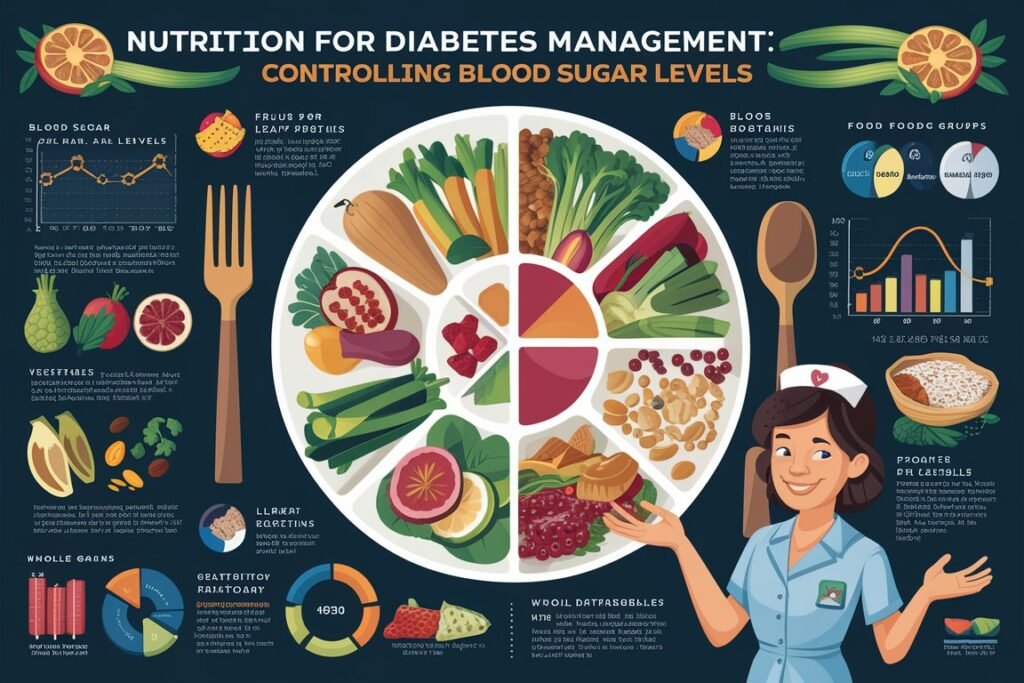
One of the key ways to manage blood sugar levels through nutrition is by paying attention to the types and amounts of carbohydrates we eat. Carbohydrates are the main nutrient that impact blood sugar levels, as they are broken down into glucose in the body. But not all carbs are created equal – some are digested and absorbed more quickly than others, leading to rapid spikes in blood sugar.
That’s where the glycemic index (GI) comes in. The GI is a measure of how quickly a particular food raises blood sugar levels compared to pure glucose. Foods with a high GI (like white bread, sugary cereals, and sweetened drinks) are digested and absorbed quickly, leading to rapid spikes in blood sugar. Foods with a low GI (like whole grains, non-starchy vegetables, and legumes) are digested and absorbed more slowly, helping to keep blood sugar levels stable.
So, one key strategy for managing blood sugar levels through nutrition is to choose more low-GI foods and fewer high-GI foods. This doesn’t mean cutting out all carbs – in fact, carbohydrates are an important part of a healthy diet for everyone, including people with diabetes. But it does mean being mindful of the types and amounts of carbs we eat, and pairing them with other nutrients like protein and healthy fats to help slow down digestion and keep blood sugar levels stable.
Nutrient-Dense Foods for Diabetes Management
In addition to paying attention to the glycemic index of foods, another key strategy for managing diabetes through nutrition is to focus on nutrient-dense, whole foods that provide a range of vitamins, minerals, and other beneficial compounds. Some examples of nutrient-dense foods that can be particularly helpful for people with diabetes include:
1. Non-Starchy Vegetables
Non-starchy vegetables like leafy greens, broccoli, cauliflower, and bell peppers are packed with fiber, vitamins, and minerals, but are low in carbohydrates and calories. Eating plenty of non-starchy veggies can help fill you up, provide important nutrients, and keep blood sugar levels stable.
2. Whole Grains
Whole grains like brown rice, quinoa, and whole wheat bread are high in fiber and other important nutrients, and have a lower glycemic index than refined grains like white rice and white bread. Choosing whole grains over refined grains can help slow down digestion and keep blood sugar levels stable.
3. Lean Proteins
Lean proteins like chicken, fish, tofu, and legumes are important for building and repairing tissues in the body, and can also help slow down digestion and keep you feeling full and satisfied. Pairing lean proteins with carbohydrates can help reduce the impact of those carbs on blood sugar levels.
4. Healthy Fats
Healthy fats like avocado, nuts, seeds, and olive oil are important for heart health and can also help slow down digestion and keep you feeling full. Choosing healthy fats over saturated and trans fats can help reduce inflammation in the body and improve overall health.
5. Low-Glycemic Fruits
While fruits contain natural sugars and can impact blood sugar levels, some fruits have a lower glycemic index than others. Low-glycemic fruits like berries, apples, and citrus fruits are high in fiber and other important nutrients, and can be a healthy choice for people with diabetes in moderation.
Meal Planning and Portion Control
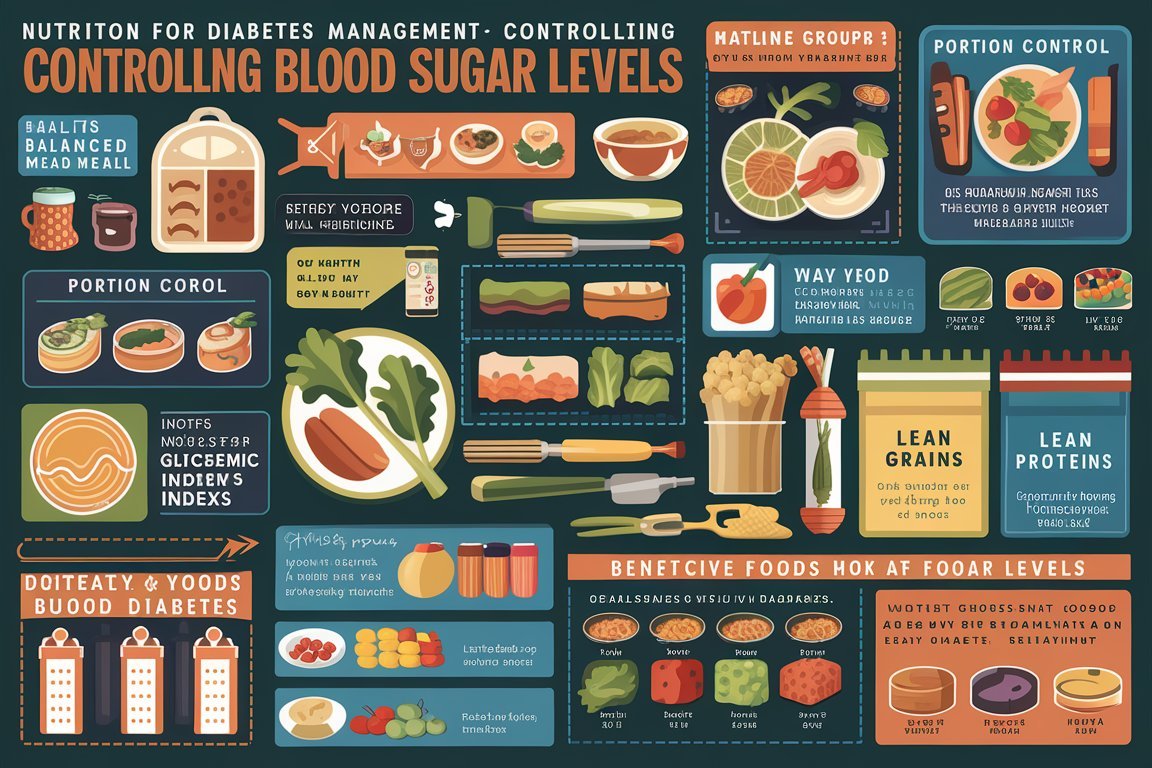
Another key aspect of managing diabetes through nutrition is paying attention to portion sizes and meal planning. Eating too much of even healthy foods can cause blood sugar levels to rise, so it’s important to be mindful of how much we’re eating at each meal and snack.
One helpful strategy for portion control is to use the “plate method.” This involves filling half of your plate with non-starchy vegetables, one-quarter with lean protein, and one-quarter with whole grains or starchy vegetables. This can help ensure that you’re getting a balance of nutrients and keeping portion sizes in check.
Meal planning can also be a helpful tool for managing diabetes through nutrition. By planning out meals and snacks in advance, you can ensure that you have healthy options on hand and avoid making impulsive food choices that may not be as good for blood sugar control. Some tips for meal planning include:
- Making a grocery list and sticking to it
- Prepping meals and snacks in advance
- Keeping healthy options like cut-up veggies and hummus, hard-boiled eggs, and unsweetened yogurt on hand for quick and easy snacks
- Experimenting with new recipes and cuisines to keep things interesting and varied
The Importance of Physical Activity
While nutrition is a key component of diabetes management, it’s important to remember that physical activity also plays a crucial role. Regular exercise can help improve insulin sensitivity, lower blood sugar levels, and reduce the risk of complications like heart disease and nerve damage.
The good news is that any type of physical activity can be beneficial for people with diabetes, whether it’s going for a walk, playing a sport, or dancing around the living room. The key is to find activities that you enjoy and can stick with long-term.
Some tips for incorporating physical activity into your diabetes management plan include:
- Setting realistic goals and starting small (like aiming for 10 minutes of activity a day and gradually building up over time)
- Finding a buddy or joining a group for accountability and support
- Mixing things up and trying new activities to keep things interesting
- Listening to your body and taking breaks when needed
Working with a Healthcare Team
Managing diabetes through nutrition and lifestyle changes can be challenging, but the good news is that you don’t have to do it alone. Working with a healthcare team that includes a registered dietitian, diabetes educator, and primary care provider can help you develop a personalized plan that meets your unique needs and goals.
A registered dietitian can help you understand how different foods impact your blood sugar levels and develop a meal plan that fits your preferences and lifestyle. They can also provide guidance on portion sizes, snacking, and dining out.
A diabetes educator can help you learn about the different aspects of diabetes management, including blood sugar monitoring, medication management, and problem-solving strategies. They can also provide support and encouragement as you navigate the challenges of living with diabetes.
Your primary care provider can help you monitor your overall health and make adjustments to your treatment plan as needed. They can also refer you to specialists like eye doctors and podiatrists to help prevent and manage potential complications.
The Bottom Line
Managing diabetes through nutrition and lifestyle changes can be a complex and ongoing process, but the benefits are well worth the effort. By focusing on nutrient-dense, low-glycemic foods, paying attention to portion sizes and meal planning, and incorporating regular physical activity, people with diabetes can improve their blood sugar control.







Leave a Reply